Before and After Image of Patient from Nevada Surgical
One of the more striking findings we see every week in our long-term follow-up clinic for patients with obesity, type 2 diabetes, and past metabolic surgery is the profound drop in triglycerides after metabolic surgery.
While elevated LDL cholesterol commonly falls over the years following metabolic surgery, the abrupt drop in triglycerides is swift and more profound. Both sleeve gastrectomy and Roux en Y gastric bypass create changes in the hormonal biochemistry of the body that result in improved lipid profile and metabolic function. While several bioactive peptides are implicated, the precise mechanism of the lipid improvements remains undetermined. Hormones GLP-1 and PYY are increased after sleeve and gastric bypass, and hormones ghrelin and leptin are reduced, perhaps offering a trail for researchers to follow, to explain lipid effects through a gut-intestine-liver-brain mechanism. We know that triglycerides fall especially reliably in animal models of sleeve and bypass, independent of weight effects, just as occurs in humans.
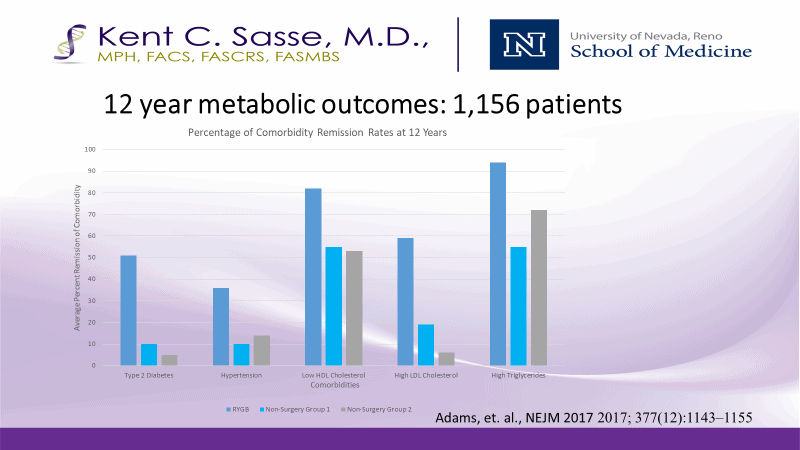
These findings are illustrated in a New England Journal of Medicine study that examined 1,156 patients including control groups of patients who did not undergo metabolic surgery. 12 years later, all metabolic parameters favored the metabolic surgery group, and most striking is the near complete resolution of hypertriglyceridemia.
Interestingly, the profound reduction in triglycerides likely adds to the factors of CV risk reduction from bariatric surgery, namely lowering LDL-C, blood pressure and Hgba1c in reducing cardiovascular risks.
Today, metabolic surgery consists of a 45-minute procedure with 4 or 5 Band-aids and a safety record better than that of appendectomy, hysterectomy or hernia repair.




