A 2018 study involving more than 17,000 patients shows a dramatic reduction in development of nephropathy and kidney failure among individuals with obesity and type 2 diabetes. When compared to standard medical management of obesity, diabetes and renal health, metabolic surgery resulted in a 3 -fold reduction in development of nephropathy over an average of 6 years.
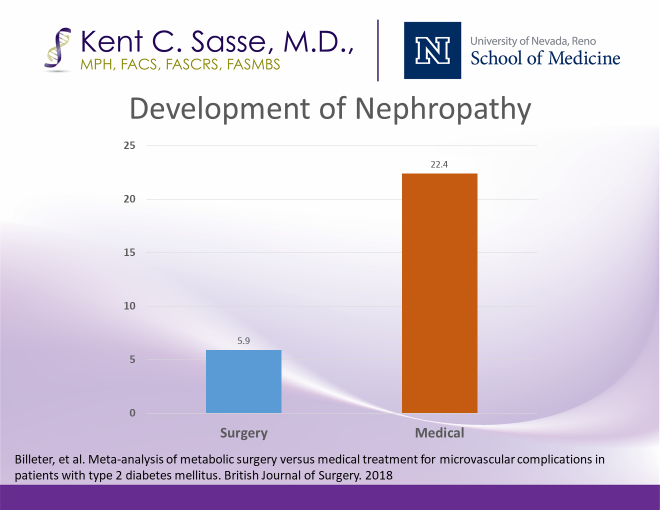
Standard medical management of diabetes and obesity has fallen woefully short of desired outcomes, with large-scale progression to nephropathy and kidney failure, and an alarming number of individuals now needing permanent dialysis. The incidence of end-stage renal disease rises annually, as depicted in the diagram below from Medicare/CMS data. Based on several studies including this recently published Billeter paper evaluating over 17,000 subjects from combined studies, many of these patients with type 2 diabetes could be spared from progression to ESRD and dialysis.
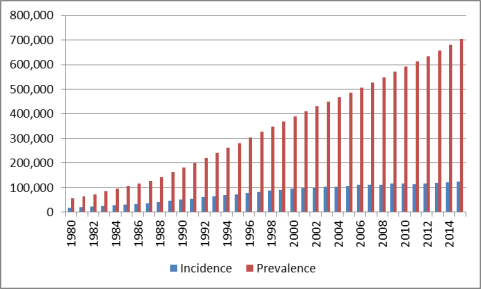
Increasing Incidence of End-stage Renal Failure in U.S.
Today, metabolic surgery consists of a 45-minute laparoscopy with risks on par with gallbladder procedures and lower than most knee, hip, C section and ventral hernia repairs. Yet patients and practitioners continue to underestimate the risks of diabetes and its microvascular complications while overestimating the risks of surgical treatment as recommended by the American Diabetes Association: metabolic surgery. When surgery is recommended by the provider for a patient with type 2 diabetes and elevated BMI, their all-cause mortality risk drops dramatically.




