Before and After Image of Patient from Nevada Surgical
Polycystic ovarian syndrome has been called a conundrum, due to its complex biology, variable symptom expression, and insufficient treatment options. The primary biology involves androgenization, infertility, obesity, and insulin resistance. Investigators have understandably seen corollaries with the biology of metabolic surgery, which counteracts such hormonal processes. A new 2020 study among sleeve gastrectomy patients adds to the numerous studies showing metabolic surgery as a safe and effective treatment, leading to resolution of infertility, hirsutism, and hyperandrogenism.
Profound impact of metabolic surgery
New research highlights the dramatic effects of bariatric surgery on increase fertility in patients with obesity and PCOS. In a 2020 publication, Singh and colleagues show sleeve gastrectomy resulted in a high rate of resolution of each element of PCOS.1 A meta-analysis of 22,000 patients showed sustained weight loss with bariatric surgery resulted in the decrease of the co-morbidities associated with obesity; resolution of diabetes occurred in 77% of cases, normalization of blood pressure occurred in 61%, and improvement of dyslipidemia in 70% of patients undergoing weight-loss surgery.1
Observational and retrospective studies show an increased rate of pregnancy and safe live births in obese patients who elect bariatric surgery. The results of these studies can be seen in the statistic that more female patients are seeking bariatric surgery at a rate of 3 females to 1 male; 70% of these females are of child-bearing age electing bariatric surgery to manage weight loss and improve fertility.2 Weight loss surgery has been demonstrated to improve menstrual irregularities; regular menstruation is achieved in >70% of anovulatory obese women undergoing bariatric surgery post-operatively.2
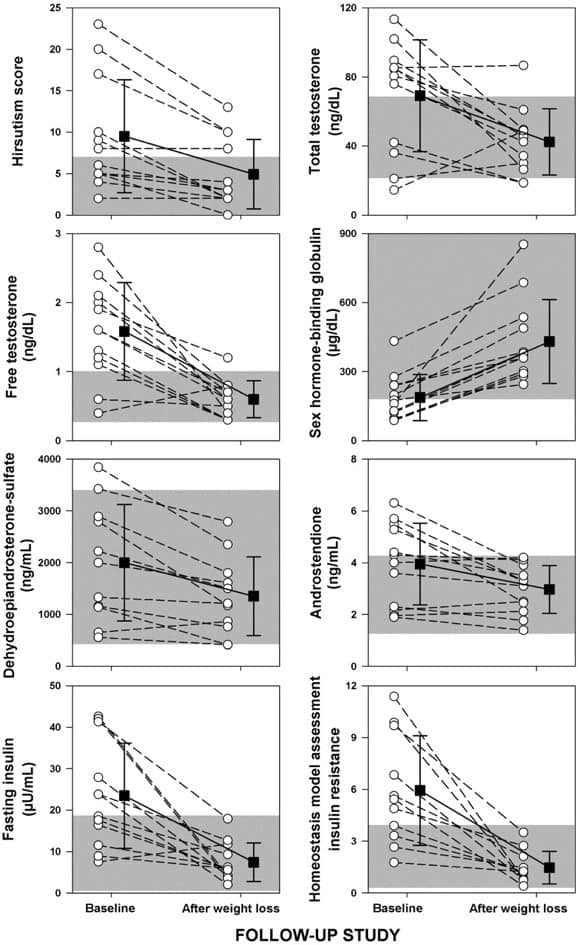
Escobar-Morreale et al.3 studied the effects on the hormone profile of obese women with PCOS undergoing metabolic surgery through a longitudinal prospective non-randomized evaluation. They found marked weight loss with complete resolution of PCOS after metabolic surgery. Hormone profiles of patients with PCOS post-operatively included recovery of ovulation and menstrual cycles, decreased insulin resistance, and hirsutism and androgen levels returned to baseline. (See Figure) Recovery of ovulation and menstrual cycles increased fecundity and subsequent pregnancies infertile women postoperatively.