Major long-term studies demonstrate diabetes remission after metabolic surgery with the sleeve gastrectomy, a 45-minute laparoscopic procedure. But patients rightly wish to know if that remission translates to meaningful gains in health and quantifiable reductions in end-organ diabetic disease, including renal, ophthalmological, and peripheral neuropathy complications.
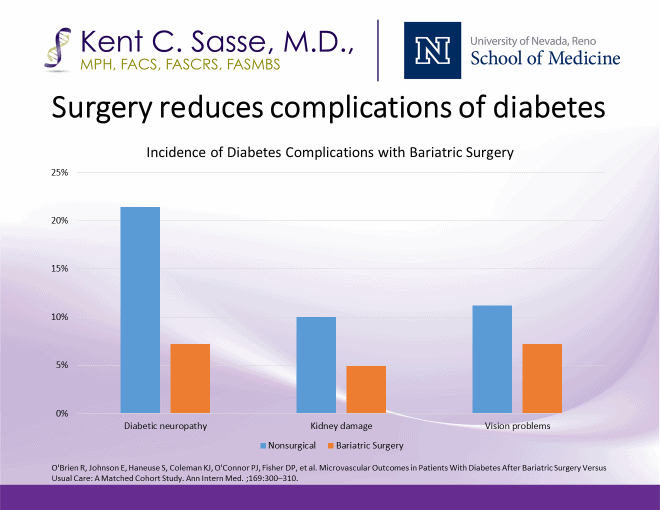
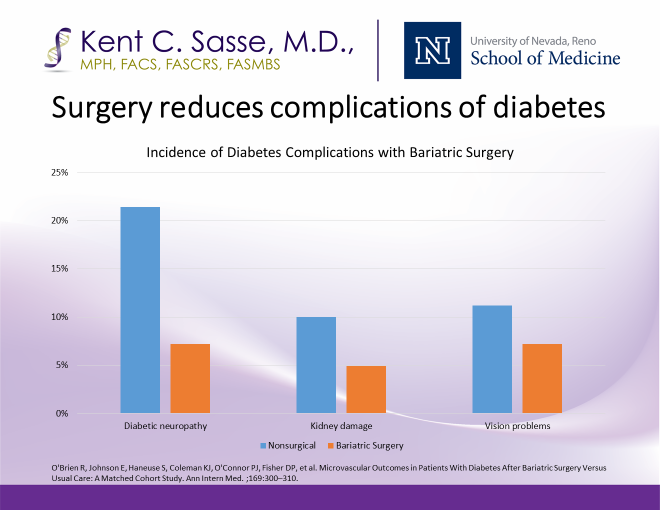
In the O’Brien matched cohort study published in the Annals of Internal Medicine, investigators studied more than 4,000 diabetic patients over a 10-year period and demonstrated large reductions in peripheral neuropathy, vision problems and diabetic nephropathy. The study confirms a “legacy effect” whereby even transient remission of diabetes lowers the long-term incidence of diabetic end-organ damage.
After surgery, most individuals with Type 2 diabetes enjoy a significant period of remission, defined by euglycemia without medications. The American Diabetes Association now recommends metabolic surgery for all patients with Type 2 diabetes and a BMI over 35.
In a previous newsletter we examined the NEJM prospective, randomized results of the 5-year STAMPEDE trial in which sleeve gastrectomy produced markedly better treatment — and in many cases total remission — of Type II diabetes when compared to intensive medical management at The Cleveland Clinic.
Such long-term data reinforce the notion of Type 2 diabetes as a complex, longitudinal disease requiring long term, multi-disciplinary care with education, exercise, lower-carbohydrate diet, medications and surgery as cornerstone treatment.
These long-term benefits come without the side effects of a bypass surgical procedure. In over 1,600 consecutive laparoscopic sleeve gastrectomy procedures, Dr. Sasse has had 0.0% mortality, and in the past 1,300 consecutive sleeve procedures over 4.5 years running, there has been 0.0% rate of the major complication of leak.
The most effective therapy for Type 2 diabetes today is a 45-minute surgical procedure.

The study authors write, “The results indicate that remission of Type 2 diabetes after bariatric surgery confers benefits for risk of incident microvascular disease even if patients eventually experience a relapse of their Type 2 diabetes. This provides support for a legacy effect of bariatric surgery, where even a transient period of surgically induced Type 2 diabetes remission is associated with lower long-term microvascular disease risk.”