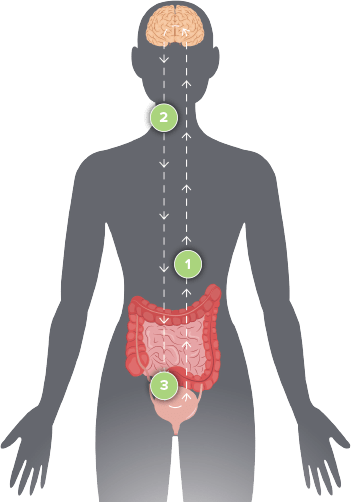
The SNM system sends gentle electrical pulses to the sacral nerves, helping to restore normal communication between the brain and bowel.
TL;DR:
- Neuromodulation therapy uses electrical pulses to correct nerve signals between the brain, spine, and bladder, thus helping manage conditions like overactive bladder, urge incontinence or urine retention.
- Two methods, Sacral Nerve Stimulation (SNS) and Tibial Nerve Stimulation (TNS), are commonly used, with FDA-approved SNS devices such as InterStim™ and Axonics Therapy™ being popular choices.
- Neuromodulation offers a balance between medications and invasive treatments, with fewer side effects and gradual improvement in nerve health.
- The devices offer extended benefits, reduced leaks, better bladder management and are often effective immediately.
- Specifically, Axonics Therapy’s device is small, rechargeable, MRI-safe and holds up to 15 years, hence avoiding frequent surgeries.
- Users may experience minor surgical side effects such as mild pain or infection risk, which typically resolve quickly.
- For women, these devices, combined with other bladder tools, present a lasting solution to bladder problems. They offer lasting control while maintaining an active lifestyle.
—
Imagine a life unburdened by bladder control issues. At the Continence Center at Nevada Surgical, we’re transforming lives with cutting-edge neuromodulation devices. These devices tap into your body’s nerve pathways, providing hope and functionality for those challenged by overactive bladders and urinary retention. As a surgeon specializing in continence, I’ve seen firsthand how this therapy can change lives. Let’s delve into the science and explore how these devices truly work. Join me in this journey to better health and well-being.
What Is Neuromodulation Therapy for Bladder Control and How Does It Work?
What is neuromodulation for bladder dysfunction?
Neuromodulation sends tiny electric pulses to nerves that help the bladder. These signals fix the connection between the brain, spine, and bladder, restoring normal flow and control.
This method helps people with overactive bladder, urge incontinence, or urine retention. It’s often used when pills fail or before full surgery. Many find peace with this therapy.
Bladder Nerve Pathways and How They Control Urine
Bladder function relies on muscle and nerve signals from the brain. The sacral nerves in the lower back play a key role. Neuromodulation uses light electric pulses to calm or activate these nerves.
We use two methods: sacral nerve stimulation (SNS) and tibial nerve stimulation (TNS).
Sacral Nerve Stimulation (SNS)
In SNS, a wire is placed near a sacral nerve at the lower back. It connects to a device that sends steady pulses. We often use the S3 nerve as it controls both the bladder and pelvic floor.
InterStim™ and Axonics Therapy™ are common SNS devices. After a trial phase, the device is placed under the skin if effective.
FDA-Approved Indications for Neuromodulation for Bladder Dysfunction
These devices are FDA-approved for:
- Overactive bladder (OAB)
- Urge incontinence
- Urinary retention
- Fecal incontinence
Who Benefits Most from Neuromodulation?
People with overactive bladder or urine retention benefit most. Neuromodulation helps those with neurologic issues too. Women may need it after birth or surgery, while men may need it after prostate work.
Neuromodulation vs Other Treatments
Neuromodulation offers a middle ground between medications and more invasive options. Unlike pills that may cause side effects, and Botox that needs repeated procedures, neuromodulation gradually enhances nerve health.
My Thoughts as a Surgeon
Neuromodulation changes lives for those with bladder issues. It’s not major surgery and has minimal downtime. Patients can try it first before making a commitment, and newer versions are long-lasting and rechargeable.
How Do Neuromodulation Devices Help Regulate Bladder Function?
What does a stimulator do for your bladder?
It sends electric pulses to calm bladder nerves and regulate signals, reducing leaks and urgency. Implant location varies, often near the sacral nerve that controls bladder muscles.
The Power of Pulses: How Electrical Signals Help
Devices mimic natural nerve signals, reducing excessive messages and boosting muscle control. This results in fewer leaks and more reliable bladder management.
Three Types of Bladder Stimulator Devices
- Implantable devices like InterStim™ and Axonics Therapy™ work under the skin with remote controls.
- External devices use office sessions, sending pulses through needles.
- Wearable models are mainly for tests or less frequent stimulation.
How We Place the Device: What Happens During the Procedure
The process starts with a trial phase to gauge results. If effective, the device is implanted under the skin. Recovery is quick, often enabling routine activities shortly after.
Famous Examples of These Devices
InterStim™ and Axonics Therapy™ lead the market. Axonics offers a rechargeable model with prolonged battery life. Both have robust results and can be MRI-safe.
How Fast Do You See Results?
Changes may be seen during the trial phase. Improvements continue with full implants, shown to be effective over years without additional interventions like meds or Botox.
What Are the Key Differences Between Axonics Therapy and Other Neuromodulation Options?
Rechargeable vs. Non-Rechargeable: How It Changes Daily Life
Axonics uses rechargeable units lasting over 15 years, which helps avoid repeated surgeries compared to Medtronic InterStim.
Device Size, Battery Life, and Being MRI-Safe
Axonics devices are small, MRI-compatible, and long-lasting, offering significant advantages over older models.
When Is Axonics Used?
Axonics is recommended for urge incontinence, urge frequency, and urinary retention, especially after other treatments fail.
How Does Axonics Compare to Medtronic InterStim?
Axonics outperforms in key aspects like size, battery life, and MRI safety. It shows high user satisfaction and reliable results in studies.
What Are the Benefits and Risks of Implantable Devices for Bladder Control?
The Pros:
- Improved bladder control and quality of life.
- Long-lasting benefits without ongoing meds.
- FNerve signal modulation without side effects like those from pills.
The Cons:
- Requires a minor surgical procedure.
- Possible mild pain or infection risk.
- Battery replacement needed eventually.
What are bladder stimulator side effects?
Side effects like mild pain or irritation typically resolve shortly after surgery. Severe issues like infection are rare but need fast attention.
How is the implant procedure done? What’s the recovery like?
The procedure is brief and recovery is quick. Patients might return to normal activities within days, with small restrictions initially.
What care does the device need later?
Implants need minimal maintenance, primarily regular battery recharging and periodic checkups with the care team.
Are these devices truly helpful?
Studies and patient experiences confirm long-term effectiveness and satisfaction, reducing leaks and urgency sustainably over years.
What Neuromodulation Options Exist Specifically for Women with Bladder Incontinence?
What types of bladder devices are made just for women?
Options include both external and implant devices like PTNS and Axonics, offering various levels of intervention without major surgery.
How do small implants help women stay active?
Devices like Axonics and InterStim are discreet, allowing full activity with minimal disruption. They provide continuous nerve regulation with user control.
What data shows these devices work better for women?
Studies indicate a high success rate among women, with notable reductions in leaks and improved quality of life over the long term.
What makes implanted bladder devices safer or better than pills?
Implanted devices present fewer side effects than medications, offering a targeted, lasting solution to bladder problems.
How does surgery for these devices compare to other bladder treatments?
These minimally invasive surgeries have distinct safety advantages over more invasive procedures, providing effective yet low-risk solutions.
Can I use a nerve device if I also use other bladder tools?
Yes, devices can be combined with pelvic floor exercises or pessaries for enhanced results, tailored to specific needs.
Final Thoughts From My Clinic Practice
Neuromodulation devices offer real improvements in bladder control, helping women lead fuller lives without constant worry about leaks. They present a smart, safe option for lasting control.
##Conclusion
Neuromodulation therapy offers hope for those with bladder issues. It works by calming bladder nerve signals, using devices like Axonics Therapy™. These implantable or external devices can change lives by reducing urgency and improving quality of life. While some risks, like infection, exist, benefits often outweigh them. Options vary from non-invasive to surgical implants, tailored for different needs and lifestyles. By understanding these therapies, you can reclaim control and comfort over your well-being.